Nov. 22, 2021 — John Farrell has mixed feelings about Thanksgiving.
“It’s great because I love eating, but by 6, 7 o’clock, I’m thinking, ‘This is not good,’” says the project manager from Virginia Beach, VA. “I’m feeling bloated, it’s feeding into the reflux. I can feel the acid coming up my throat, that burning sensation. There’s a lot of regret about everything I did that day.”
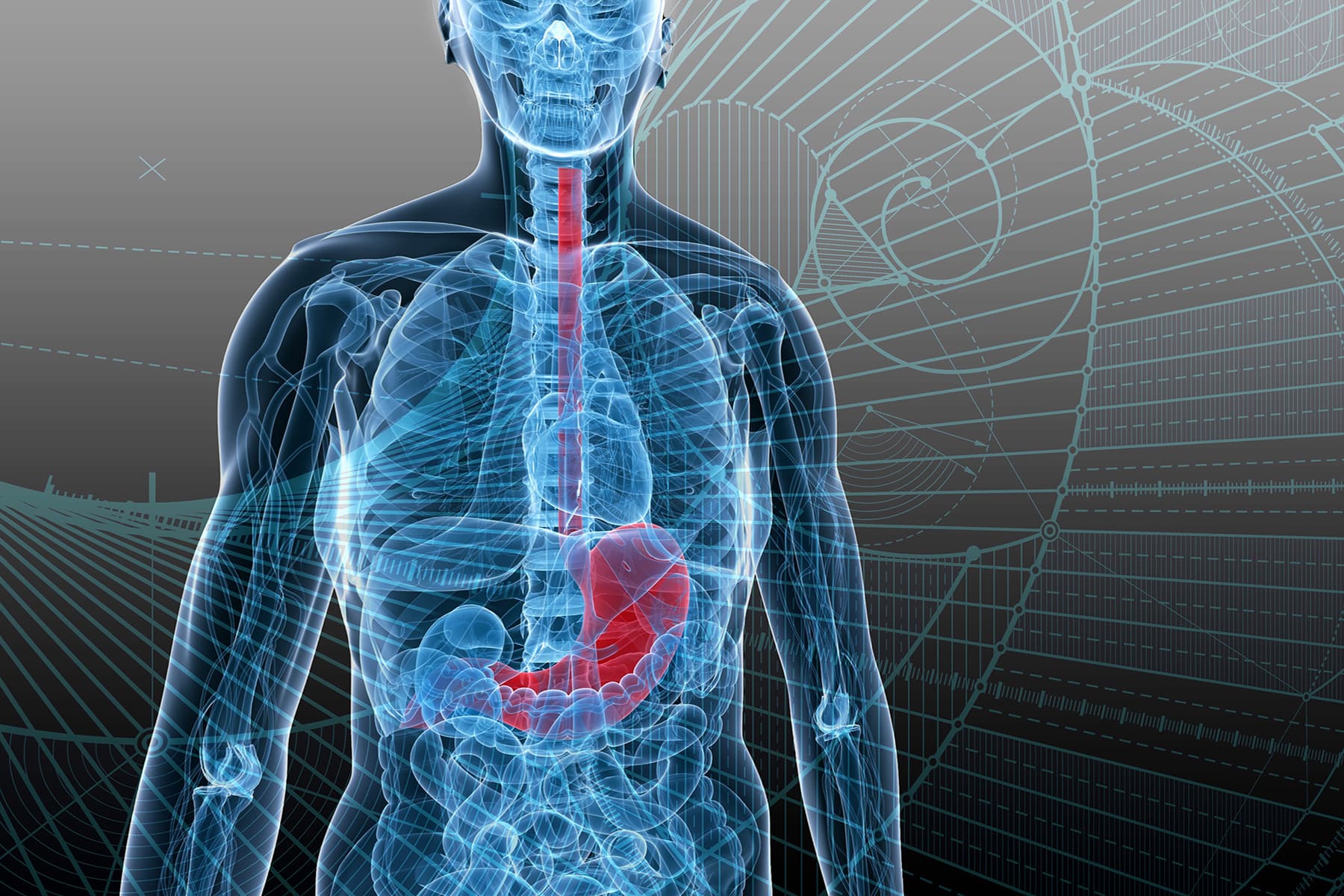
For around 5 years, Farrell, 46, has had GERD, which stands for gastroesophageal reflux disease. With this digestive disorder, your lower esophageal sphincter (LES, a muscular valve between your esophagus and your stomach) doesn’t work properly. It lets food and stomach acids reflux — flow back up — into your esophagus, which can cause discomfort and a burning sensation.
Most of us have occasional periods of reflux and the heartburn that can result, but with GERD, it happens two or more times a week. Roughly 60 million Americans have heartburn at least once a month, and as many as 15 million experience it daily. If GERD goes untreated, it can cause much worse symptoms and even lead to esophageal cancer.
While you may have heard that spicy, fatty, or rich foods should be avoided to prevent acid reflux, the reality is more complicated than that.
“Every individual has a different trigger for their GERD,” says Rena Yadlapati, MD, director of the Center for Esophageal Diseases at the University of California-San Diego. “I have some patients that can eat spicy, spicy foods, but they get reflux when they eat chocolate. I have others that just cannot drink coffee, but any food is just fine.”
Stefanie Robinson, a medical and dental biller from Pleasant Valley, NY, knows her triggers: acidic foods like tomatoes, and stress. She’s been struggling with GERD on and off for 20 years.
“I take [acid-reducing drug] omeprazole every night,” she says. “Lately I’ve been feeling stressed, so it doesn’t seem to be doing much. I take Tums in between. And rice pudding or yogurt will help settle my stomach — they seem to coat it.”
In addition to spicy foods and tomato products, Farrell says he has two other key triggers: overeating and lying down too soon.
“The most important things with GERD are the amount of food you eat, and the relationship with sleeping,” Yadlapati says. “It takes a few hours for the stomach to empty down into the small bowels. Once the stomach has emptied, you really don’t have a risk of having reflux from the stomach. But until then, whatever is in the stomach is likely to come back up.”
Thanksgiving poses particular challenges for people with GERD, for one simple reason: “GERD is all about pressure,” Yadlapati says. “The more pressure we have in our stomach, the more likely reflux is to be triggered. And the thing that causes pressure is large amounts of food.”
Other things related to the holiday, like the stress of travel and family gatherings, may make you more prone to an attack, she says.
“Stress increases the excitability of nerves in your esophagus. If you’re having small amounts of reflux, on any other day, that might not cause symptoms. But under stressful circumstances, it might cause severe chest pain and burning.”
Another common part of holiday celebrations can also cause trouble.
“Alcohol is known to relax the lower esophageal sphincter, which facilitates reflux,” says Allon Kahn, MD, an assistant professor of medicine at the Mayo Clinic in Scottsdale, AZ. “So it’s likely, especially in the presence of a big meal, to make symptoms worse.”
While some people who have GERD take medication to help them produce less stomach acid, others manage with lifestyle changes like identifying and avoiding trigger foods or waiting at least 3 hours after eating to lie down. But on Thanksgiving, those careful practices often go out the window. Letting loose can lead to a nasty bout of GERD.
“Patients who are controlled with medicine might be less likely to have worsening of their symptoms, because the acid has been reduced to the point where it may not bother them as much,” says Kahn.
Whether you know you have GERD or you just get heartburn occasionally, a few tips can help you pull off a pain-free Thanksgiving:
Even with the best of intentions, you may still find yourself in pain Thanksgiving night. Here’s what you can do:
John Farrell, Virginia Beach, VA.
American College of Gastroenterology: “Acid Reflux.”
NIH MedlinePlus: “Heartburn: What you need to know.”
Rena Yadlapati, MD, associate professor of medicine, director, Center for Esophageal Diseases, University of California-San Diego.
Stefanie Robinson, Pleasant Valley, NY.
Allon Kahn, MD, assistant professor of medicine, Division of Gastroenterology & Hepatology, Mayo Clinic, Scottsdale, AZ.
© 2005 – 2022 WebMD LLC. All rights reserved.
WebMD does not provide medical advice, diagnosis or treatment.
See additional information.